What is Home Enteral Nutrition? Understanding Benefits, Risks, and More. Discover what home enteral nutrition is, its benefits, potential risks, and how it compares to other forms of nutrition support. Learn everything you need to know about home enteral nutrition here.
Introduction

Transitioning to home enteral nutrition can significantly improve the quality of life for individuals needing long-term nutritional support. It allows patients to receive necessary nutrients in the comfort of their homes, ensuring continuity of care and promoting independence.
What is Home Enteral Nutrition?

Home enteral nutrition (HEN) involves delivering liquid nutrition directly to the stomach or small intestine through a tube. This method is essential for individuals who cannot consume food orally but need sufficient nutrition to maintain their health.
Benefits of Home Enteral Nutrition
- Improved Quality of Life: Patients can stay in their familiar home environment, promoting emotional and psychological well-being.
- Reduced Hospital Stays: Home enteral nutrition minimizes the need for prolonged hospitalizations, decreasing the risk of hospital-acquired infections.
- Personalized Nutrition: Patients receive tailored nutritional support that meets their specific dietary needs and medical conditions.
- Cost-Effective: Home enteral nutrition is often more affordable than long-term hospital care, saving on medical expenses.
- Enhanced Mobility: Patients can maintain a more active lifestyle, as home enteral nutrition allows for greater freedom and flexibility.
- Family Involvement: Families can participate in the care process, providing support and improving patient morale.
- Consistency in Care: Patients benefit from continuous, uninterrupted nutritional support, ensuring better health outcomes.
- Convenience: Home enteral nutrition is more convenient for patients and their families, eliminating the need for frequent hospital visits.
- Customized Feeding Schedules: Patients can follow feeding schedules that fit their daily routines and preferences.
- Decreased Healthcare Burden: Reduces the demand on hospital resources and healthcare providers, allowing them to focus on acute care needs.
Comparison of Home Enteral Nutrition vs. Hospital-Based Enteral Nutrition in Terms of Patient Independence
| Aspect | Home Enteral Nutrition | Hospital-Based Enteral Nutrition |
|---|---|---|
| Location of Care | Administered at home, providing a comfortable setting. | Administered in a clinical or hospital environment. |
| Patient Mobility | Higher mobility and freedom to move around. | Limited mobility due to hospital protocols and setting. |
| Daily Routine | Allows patients to maintain their normal daily routines. | Routines are structured around hospital schedules. |
| Family Involvement | Families can actively participate in care. | Limited family involvement due to hospital restrictions. |
| Healthcare Supervision | Remote monitoring with periodic professional check-ins. | Continuous, direct supervision by healthcare staff. |
Analysis
- Enhanced Comfort: Home enteral nutrition offers a familiar and comfortable environment, promoting patient independence.
- Greater Freedom: Patients experience higher mobility and the ability to move freely, unlike the restrictions in a hospital setting.
- Maintained Routines: Patients can follow their personal daily routines, enhancing their sense of normalcy and control.
- Active Family Role: Family members can provide daily support and care, increasing patient comfort and involvement.
- Balanced Supervision: While remote monitoring is sufficient, patients still receive necessary healthcare support without constant supervision, fostering independence.
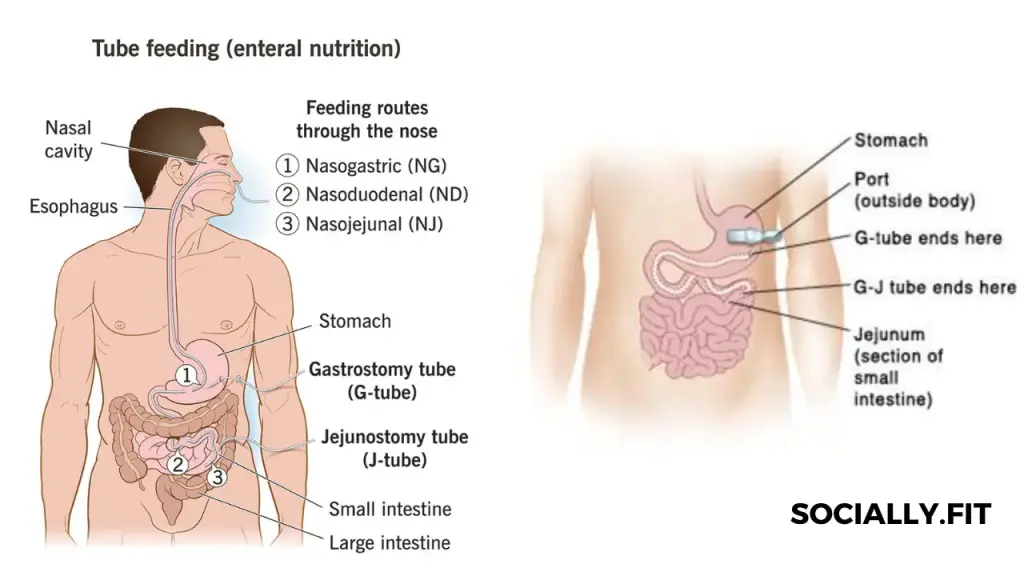
Types of Enteral Nutrition

- Nasogastric Tube (NG Tube): Inserted through the nose and extends to the stomach, suitable for short-term feeding.
- Orogastric Tube: Similar to the NG tube but inserted through the mouth, often used in infants or when nasal insertion is not possible.
- Gastrostomy Tube (G-Tube): Surgically placed directly into the stomach through the abdominal wall, ideal for long-term nutrition.
- Jejunostomy Tube (J-Tube): Inserted into the jejunum (part of the small intestine) via the abdominal wall, used when the stomach must be bypassed.
- Nasoduodenal Tube: Extends from the nose to the duodenum (first part of the small intestine), used when feeding into the stomach is not feasible.
- Percutaneous Endoscopic Gastrostomy (PEG): A type of G-tube placed endoscopically, less invasive than surgical placement.
- Button Gastrostomy Device: A low-profile G-tube that sits flush against the skin, offering more comfort and discretion for long-term feeding.
Comparison of Infection Risk: Home Enteral Nutrition vs. Traditional Oral Feeding in Patients with Compromised Immunity
| Aspect | Home Enteral Nutrition | Traditional Oral Feeding |
|---|---|---|
| Site Infection | Higher risk due to feeding tube insertion site | No risk as no tube insertion is required |
| Gastrointestinal Infections | Possible risk if formula contamination occurs | Lower risk with proper food handling |
| Respiratory Infections | Reduced risk as aspiration is minimized | Increased risk if swallowing difficulties present |
| Overall Hygiene | Requires strict hygiene practices to prevent infections | Standard hygiene practices suffice |
| Healthcare Monitoring | Periodic professional monitoring helps manage risks | Routine visits; less frequent infection monitoring needed |
Analysis
- Site Infection Control: Home enteral nutrition demands rigorous care of the insertion site to prevent infections, unlike oral feeding which has no such requirement.
- Preventing Contamination: Ensuring the formula is uncontaminated is crucial for home enteral nutrition, whereas oral feeding mainly requires safe food preparation.
- Minimized Aspiration Risk: Home enteral nutrition lowers the risk of respiratory infections by reducing aspiration incidents compared to oral feeding, which can pose a risk for those with swallowing difficulties.
- Hygiene Standards: Maintaining higher hygiene standards is vital for home enteral nutrition, preventing infection, unlike the standard hygiene needed for traditional feeding.
- Regular Monitoring: Home enteral nutrition benefits from regular professional check-ins to manage infection risks, while traditional oral feeding typically involves less frequent monitoring.
Potential Risks and Complications of Home Enteral Nutrition

- Tube Dislodgement: The feeding tube can become dislodged, requiring medical intervention to reposition or replace it.
- Infection: The insertion site can become infected if not properly cared for, necessitating strict hygiene practices.
- Blockages: The tube can become blocked by formula or medication, requiring regular flushing to maintain patency.
- Gastrointestinal Issues: Patients may experience diarrhea, constipation, or bloating, needing adjustments in formula or feeding schedule.
- Aspiration: There is a risk of formula entering the lungs, particularly if the patient is not positioned correctly during feeding.
- Skin Irritation: The area around the insertion site can become irritated or develop pressure sores, needing frequent assessment and care.
- Nutritional Imbalance: Inadequate or excessive nutrient delivery can occur, necessitating regular monitoring and adjustments.
- Tube Deterioration: Over time, the tube material can degrade, requiring periodic replacement to ensure proper function.
- Mechanical Failures: Issues with the feeding pump or other equipment can disrupt feeding schedules, needing prompt technical support.
- Emotional Stress: Both patients and caregivers may experience stress or anxiety related to the complexities of home enteral nutrition, requiring emotional and psychological support.
Comparison of Managing Complications: Home Enteral Nutrition vs. Parenteral (Intravenous) Nutrition
| Aspect | Home Enteral Nutrition | Parenteral (Intravenous) Nutrition |
|---|---|---|
| Infection Risk Management | Focus on preventing site infections at the tube insertion site through strict hygiene practices. | Focus on preventing bloodstream infections through aseptic techniques and central line care. |
| Nutritional Monitoring | Regular assessment of formula tolerance and nutrient absorption. | Frequent monitoring of blood nutrient levels to adjust IV formulations. |
| Mechanical Complications | Dealing with tube blockages, dislodgements, and pump failures. | Managing catheter occlusions, line displacements, and pump malfunctions. |
| Gastrointestinal Issues | Monitoring and managing diarrhea, constipation, and bloating. | No direct gastrointestinal issues, but must monitor for liver complications due to prolonged IV nutrition. |
| Patient Mobility | High mobility, allowing patients to move freely with proper tube care. | Limited mobility due to the need to stay connected to IV lines and infusion pumps. |
Analysis
- Infection Control: Home enteral nutrition primarily involves preventing infections at the tube site, whereas parenteral nutrition focuses on preventing serious bloodstream infections.
- Nutritional Adjustments: Enteral nutrition requires monitoring the patient’s response to the formula, adjusting as needed, while parenteral nutrition involves frequent blood tests to tailor the IV solution.
- Addressing Blockages: Tube blockages and mechanical failures are common in enteral nutrition, needing routine maintenance, whereas parenteral nutrition deals with catheter-related issues.
- Digestive Health: Enteral nutrition patients may face gastrointestinal complications needing management, unlike parenteral nutrition, which bypasses the digestive system but can affect liver function.
- Patient Activity: Enteral nutrition supports greater patient mobility, enhancing quality of life, whereas parenteral nutrition often restricts movement due to the complexity of managing IV lines.
Frequently Asked Questions (FAQs)

- What is the primary purpose of home enteral nutrition?
- Home enteral nutrition provides necessary nutrients to individuals who cannot eat orally.
- How is the feeding tube maintained?
- The feeding tube requires regular flushing with water to prevent blockages and routine cleaning to avoid infections.
- Can patients travel while on home enteral nutrition?
- Yes, with proper planning and equipment, patients can travel while receiving home enteral nutrition.
- Are there different formulas for enteral nutrition?
- Yes, formulas vary based on caloric needs, digestive capability, and specific nutritional requirements.
- What should one do if there is a problem with the feeding tube?
- Contact a healthcare professional immediately for guidance and support if there are any issues with the feeding tube.
Conclusion
In conclusion, home enteral nutrition serves as a vital lifeline for individuals who cannot consume food orally but require essential nutrients for their well-being. By delivering liquid nutrition directly to the stomach or small intestine through a tube, home enteral nutrition enables patients to receive tailored nutritional support in the comfort of their own homes. This approach not only promotes independence and enhances quality of life but also reduces the need for prolonged hospital stays, minimizing the risk of hospital-acquired infections. Despite the potential risks and complications associated with home enteral nutrition, such as infection and tube-related issues, careful management and adherence to medical guidelines can mitigate these challenges. Overall, home enteral nutrition plays a crucial role in ensuring the nutritional needs and overall health of patients with diverse medical conditions are met effectively.